The COVID Turning Point: How Fauci and Public Health Lost Their Scientific Compass
Science
2025-04-05 19:08:17Content

Five years have passed since the unprecedented COVID-19 pandemic dramatically reshaped our world. Looking back to April 2020, we can now reflect on the tumultuous period when mask recommendations first emerged, largely influenced by the Centers for Disease Control and Prevention's (CDC) initial response to the global health crisis.
Those early months were characterized by uncertainty, fear, and rapid adaptation. The CDC's guidance, while well-intentioned, was often perceived as inconsistent and confusing. As communities grappled with an invisible threat, mask-wearing became a symbol of collective resilience and personal responsibility.
Today, we've gained valuable perspective on those challenging times. The pandemic exposed critical vulnerabilities in our healthcare systems, social structures, and global preparedness. It also highlighted the remarkable human capacity for innovation, compassion, and adaptation in the face of unprecedented challenges.
While the memories of those intense months remain vivid, we've emerged with a deeper understanding of public health, community support, and the importance of scientific collaboration. The COVID-19 era serves as a powerful reminder of our interconnectedness and the critical role of informed, coordinated responses during global health emergencies.
Unmasking the Pandemic Paradox: A Critical Examination of COVID-19 Response
In the tumultuous landscape of global health crisis management, few events have sparked as much controversy and introspection as the COVID-19 pandemic. The unprecedented challenges faced by public health institutions, particularly the Centers for Disease Control and Prevention (CDC), have raised critical questions about crisis response, scientific communication, and institutional credibility.Navigating Uncertainty: When Science Meets Public Panic
The Origins of Institutional Uncertainty
The COVID-19 pandemic exposed profound vulnerabilities within public health infrastructure, challenging long-held assumptions about emergency preparedness. As the virus swept across continents, health institutions found themselves navigating uncharted territories, wrestling with rapidly evolving scientific understanding and immense public pressure. The CDC, traditionally viewed as a beacon of scientific guidance, suddenly found itself at the epicenter of a complex and unpredictable global health emergency. Institutional decision-making became a high-stakes balancing act between scientific caution and public communication. Recommendations shifted dramatically, creating a landscape of confusion and skepticism. The implementation of mask mandates represented a particularly contentious aspect of pandemic response, highlighting the delicate interplay between scientific evidence and public perception.Psychological Dimensions of Pandemic Response
The collective psychological impact of COVID-19 interventions cannot be understated. Mass masking represented more than a medical intervention; it became a complex social phenomenon that transformed interpersonal interactions, public spaces, and individual perceptions of safety. Sociological research suggests that such widespread behavioral modifications trigger profound psychological responses, ranging from heightened anxiety to a sense of collective resilience. Behavioral scientists observed intricate patterns of compliance, resistance, and adaptation. The mask became a powerful symbol, transcending its medical utility to represent individual beliefs, political affiliations, and personal interpretations of risk. This symbolic transformation revealed deeper societal fractures and communication challenges within public health frameworks.Scientific Communication in Crisis
The pandemic highlighted critical gaps in scientific communication strategies. Institutional responses were frequently characterized by uncertainty, evolving recommendations, and communication challenges that eroded public trust. The CDC's messaging struggled to balance scientific nuance with clear, actionable guidance, creating an environment of confusion and skepticism. Transparency became a crucial yet challenging objective. Each revised recommendation, each modified protocol, potentially undermined institutional credibility. The delicate balance between acknowledging scientific uncertainty and providing confident guidance proved extraordinarily complex, exposing systemic communication vulnerabilities.Long-Term Institutional Implications
The COVID-19 response will likely be studied for decades as a pivotal moment in public health history. Institutional learning became paramount, with organizations critically examining their crisis response mechanisms, communication strategies, and adaptability. The pandemic served as an unprecedented stress test for global health infrastructure, revealing both remarkable resilience and significant structural weaknesses. Future preparedness demands a fundamental reimagining of crisis response protocols. Institutions must develop more agile, transparent, and adaptable frameworks that can rapidly integrate emerging scientific understanding while maintaining public confidence. The lessons learned extend far beyond pandemic management, touching fundamental aspects of scientific communication and institutional trust.Technological and Social Transformation
COVID-19 accelerated technological and social transformations that will resonate for generations. Remote work, digital communication, and technology-mediated social interactions became normalized, fundamentally reshaping societal structures. Public health interventions catalyzed innovations in healthcare, education, and workplace dynamics, demonstrating humanity's remarkable capacity for adaptation. The pandemic experience underscored the interconnectedness of global systems, highlighting how individual actions and institutional responses are intrinsically linked. Each decision, each recommendation carried profound ripple effects that transcended immediate medical considerations.RELATED NEWS
Science

Ideological Warfare: Dugin's Bold Crusade to Decolonize Russian Academic Thought
2025-02-25 08:09:53
Science

Science in Peril: NIH Budget Cuts Could Unravel Decades of Research Breakthroughs
2025-04-17 18:05:00
Science
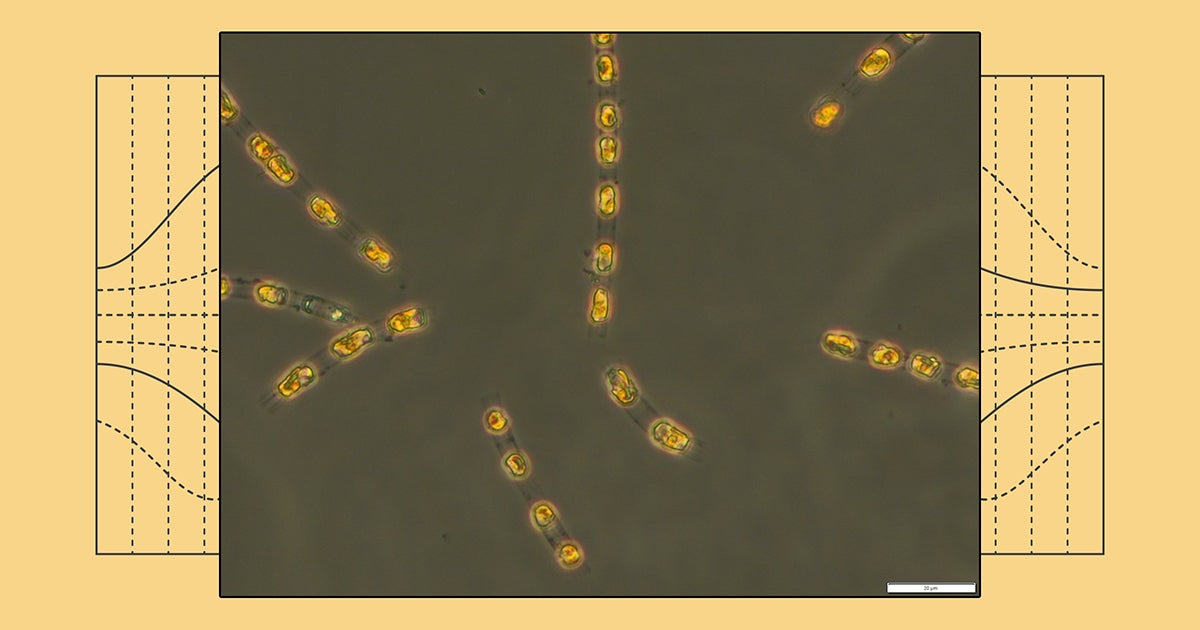
Deep-Sea Resurrection: Ancient Microbe Awakens After Millennia in Oceanic Darkness
2025-04-13 20:30:24