Breaking: State Lawmakers Fast-Track Healthcare Reform to Cut Red Tape
Health
2025-05-02 17:31:05Content
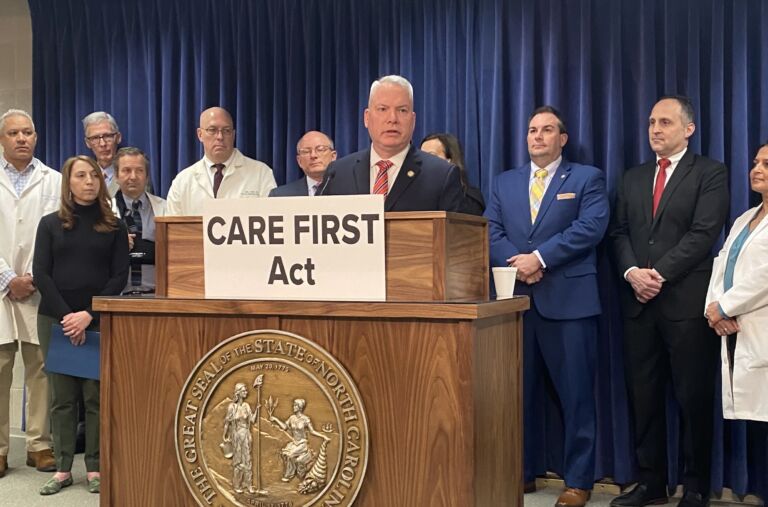
In a dynamic legislative session, the North Carolina General Assembly made significant strides this week, pushing forward a series of pivotal health care bills that promise to reshape the state's medical landscape. Lawmakers focused on key areas including Medicaid work requirements, providing much-needed regulatory relief for hospitals, and implementing comprehensive health care reforms.
The proposed legislation signals a proactive approach to addressing complex healthcare challenges, with potential implications for both healthcare providers and residents across North Carolina. By targeting critical areas such as Medicaid eligibility, hospital administrative processes, and systemic healthcare improvements, the General Assembly demonstrates its commitment to enhancing the state's healthcare ecosystem.
These bills represent a nuanced attempt to balance cost-effectiveness, patient access, and institutional flexibility, reflecting the ongoing evolution of healthcare policy in the state. As the proposals move through the legislative process, stakeholders are closely watching their potential impact on medical services, patient care, and overall health system efficiency.
North Carolina's Healthcare Landscape: A Transformative Legislative Journey
In the dynamic realm of healthcare policy, the North Carolina General Assembly has emerged as a pivotal force, driving substantial reforms that promise to reshape the state's medical ecosystem. As legislative mechanisms churn, healthcare stakeholders find themselves at the cusp of potentially groundbreaking changes that could redefine patient access, provider regulations, and systemic healthcare delivery.Navigating the Complex Terrain of Healthcare Reform: What Lies Ahead?
Medicaid Work Requirements: Balancing Accessibility and Accountability
The proposed Medicaid work requirements represent a nuanced approach to healthcare entitlement, challenging traditional welfare paradigms. Policymakers are meticulously crafting legislation that seeks to create a delicate equilibrium between social support and individual responsibility. By implementing structured work mandates, the General Assembly aims to incentivize economic participation while maintaining a robust safety net for vulnerable populations. Comprehensive analysis reveals that these requirements are not merely punitive measures but strategic interventions designed to promote self-sufficiency. Healthcare experts argue that such policies could potentially reduce long-term dependency, encourage skill development, and create pathways to economic mobility for Medicaid recipients.Hospital Regulatory Relief: Streamlining Institutional Frameworks
The legislative agenda demonstrates a profound commitment to alleviating regulatory burdens confronting healthcare institutions. By proposing targeted regulatory relief, the General Assembly acknowledges the complex challenges hospitals face in an increasingly complex healthcare landscape. These proposed reforms aim to reduce administrative overhead, potentially allowing medical facilities to redirect resources toward patient care, technological innovation, and infrastructure improvements. The strategic approach suggests a nuanced understanding of the intricate balance between regulatory oversight and institutional flexibility.Comprehensive Health Care Reforms: A Holistic Transformation
Beyond isolated policy interventions, the General Assembly is orchestrating a comprehensive reimagining of healthcare delivery. The proposed reforms extend far beyond surface-level modifications, promising a fundamental restructuring of how medical services are conceptualized, accessed, and delivered. Stakeholders anticipate that these reforms could potentially address long-standing systemic inefficiencies, improve patient outcomes, and create more responsive healthcare ecosystems. The multifaceted approach indicates a sophisticated understanding of the interconnected nature of healthcare policy, economic considerations, and social welfare.Economic and Social Implications: A Broader Perspective
The proposed legislative changes transcend traditional healthcare policy boundaries, presenting profound economic and social implications. By reimagining Medicaid structures, hospital regulations, and systemic healthcare frameworks, North Carolina positions itself as a potential model for innovative policy development. Economic analysts suggest that these reforms could generate significant downstream effects, potentially stimulating job creation, improving workforce participation, and creating more sustainable healthcare infrastructure. The holistic approach demonstrates a forward-thinking strategy that considers long-term societal impacts.Technological and Infrastructural Considerations
Underlying these legislative efforts is a recognition of technological transformation's critical role in modern healthcare delivery. The proposed reforms implicitly acknowledge the need for adaptive, technology-enabled healthcare systems that can respond dynamically to emerging challenges. From potential digital infrastructure improvements to more flexible regulatory frameworks, the legislative agenda suggests a commitment to creating an environment conducive to technological innovation and efficient healthcare service delivery.RELATED NEWS
Health

Medical Mavericks: UVA Health Team Clinches Breakthrough in STAT Madness Showdown
2025-03-10 12:25:00
Health
Mental Health Care Gets Boost: Lawmakers Push for Higher University Clinic Payments
2025-04-04 11:55:04






