Health Divided: The Myth of America's Wellness Utopia
Health
2025-04-24 08:33:54Content

A Nation's True Health: Confronting Persistent Inequalities
The measure of a country's well-being extends far beyond simple health statistics. When disparities continue to plague specific population segments year after year, it reveals a deeper, more troubling narrative about societal inequity. These persistent gaps in health outcomes are not just numbers on a page—they represent real lives impacted by systemic challenges.
True national health is not about averages, but about ensuring every citizen has equitable access to healthcare, resources, and opportunities. When certain communities consistently experience lower health outcomes, it exposes critical fractures in the social infrastructure. These disparities—whether related to income, race, geography, or education—create a complex web of challenges that cannot be ignored.
Addressing these inequalities requires more than surface-level interventions. It demands a comprehensive approach that tackles root causes: improving access to quality healthcare, addressing socioeconomic barriers, and creating targeted support systems for marginalized communities. Only by recognizing and actively working to eliminate these disparities can a nation truly claim to be healthy.
The path to genuine national well-being lies in our collective commitment to equity, understanding that a society is only as strong as its most vulnerable members. Until we bridge these persistent gaps, our vision of national health remains incomplete and fundamentally compromised.
Unmasking Societal Inequities: A Deep Dive into National Health Disparities
In the intricate tapestry of national well-being, health disparities represent more than just statistical anomalies—they are profound indicators of systemic challenges that penetrate the very core of social infrastructure. These persistent inequalities reveal deep-rooted structural issues that demand comprehensive examination and transformative action.Breaking the Cycle of Systemic Health Inequalities: A Critical National Challenge
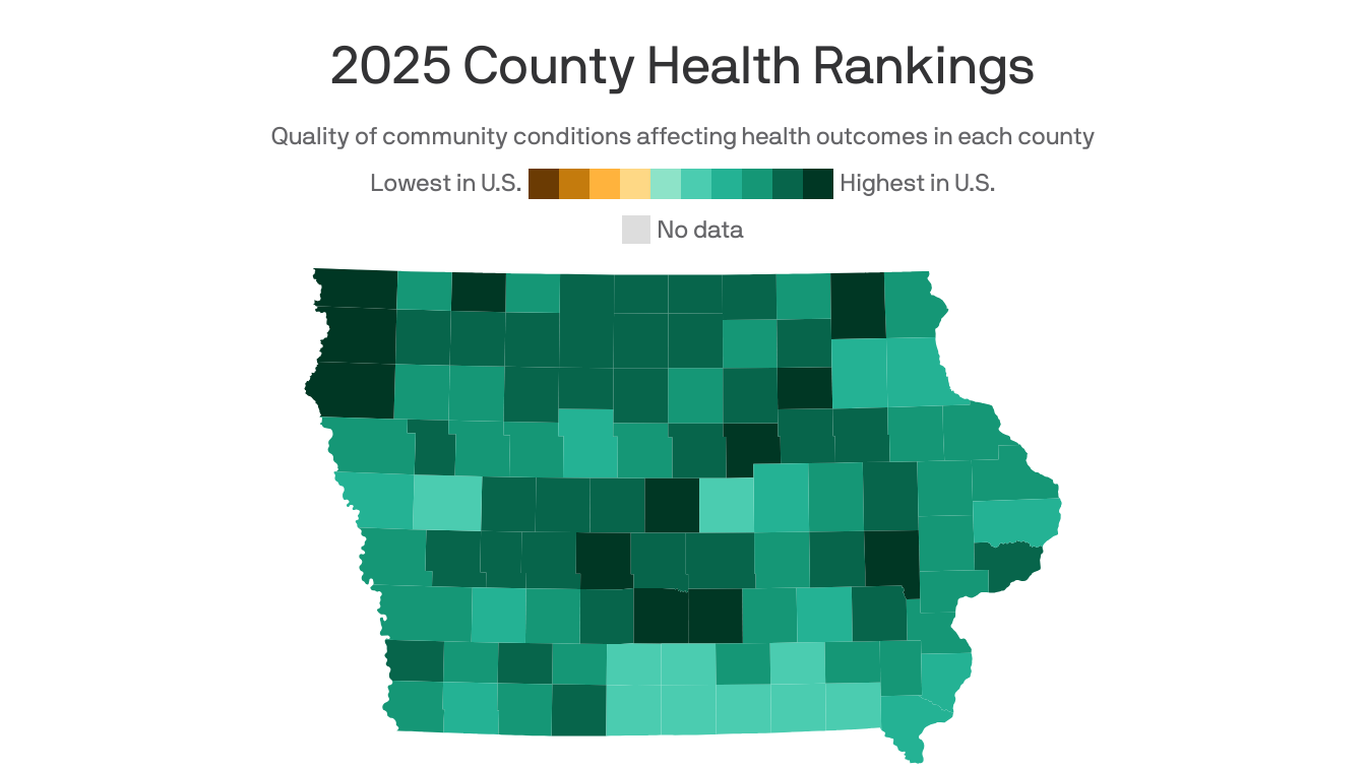
The Anatomy of Health Disparities
The landscape of national health is a complex ecosystem where socioeconomic factors, racial backgrounds, geographic locations, and access to resources intersect to create intricate patterns of wellness and vulnerability. Researchers have long observed that certain population segments consistently experience disproportionate health challenges, suggesting systemic barriers that extend far beyond individual circumstances. These disparities manifest in multiple dimensions—from healthcare access and quality of medical treatment to preventative care opportunities and long-term health outcomes. The persistent nature of these inequalities indicates deeply embedded structural challenges that require multifaceted interventions.Socioeconomic Roots of Health Inequity
Economic stratification plays a pivotal role in determining health trajectories. Communities with limited financial resources often encounter significant obstacles in accessing comprehensive healthcare services. This economic marginalization translates into reduced preventative care, delayed medical interventions, and ultimately, compromised health outcomes. The correlation between economic status and health is not coincidental but a direct consequence of systemic inequalities. Lower-income populations frequently experience higher stress levels, limited nutritional options, and environments that inherently pose greater health risks. These compounding factors create a cyclical pattern of health disadvantage that becomes increasingly challenging to disrupt.Racial and Ethnic Dimensions of Healthcare Accessibility
Racial and ethnic minorities continue to experience substantial healthcare disparities that reflect broader societal inequities. Historical patterns of discrimination, institutional racism, and systemic barriers contribute to significantly different health experiences across demographic groups. Medical research has consistently demonstrated that minority populations often receive suboptimal medical care, experience higher rates of chronic diseases, and encounter more significant challenges in accessing quality healthcare services. These disparities are not merely statistical anomalies but represent profound systemic failures that demand comprehensive policy interventions.Technological and Infrastructural Challenges
The digital divide and technological infrastructure further exacerbate existing health disparities. Rural and economically marginalized communities frequently lack advanced medical facilities, telemedicine options, and comprehensive health information networks. This technological gap translates into reduced healthcare accessibility, limited medical knowledge dissemination, and decreased opportunities for preventative and specialized medical interventions. The geographical and technological barriers create additional layers of complexity in addressing national health inequities.Policy Implications and Transformative Strategies
Addressing national health disparities requires a holistic approach that transcends traditional medical frameworks. Policymakers must develop comprehensive strategies that integrate healthcare, economic development, educational opportunities, and social support systems. Targeted investments in community health infrastructure, culturally sensitive medical training, and equitable resource allocation can potentially mitigate existing disparities. Moreover, data-driven policy interventions that recognize the nuanced experiences of different population segments can create more responsive and inclusive healthcare ecosystems.The Path Forward: Collaborative Transformation
Resolving national health disparities demands unprecedented collaboration between government institutions, healthcare providers, community organizations, and academic research centers. By fostering interdisciplinary approaches and centering marginalized experiences, societies can develop more responsive and equitable health frameworks. The journey toward health equity is not merely a medical challenge but a profound social transformation that requires sustained commitment, empathy, and innovative thinking. Each step toward addressing these disparities represents a critical investment in collective national well-being.RELATED NEWS
Health

Brain Boost: Neurologists Reveal 10 Surprising Tricks to Sharpen Your Mind
2025-04-03 09:00:27
Health

Patient Safety Champions: Kettering Health Scores Top Marks in Nationwide Hospital Evaluation
2025-05-01 15:15:11
Health
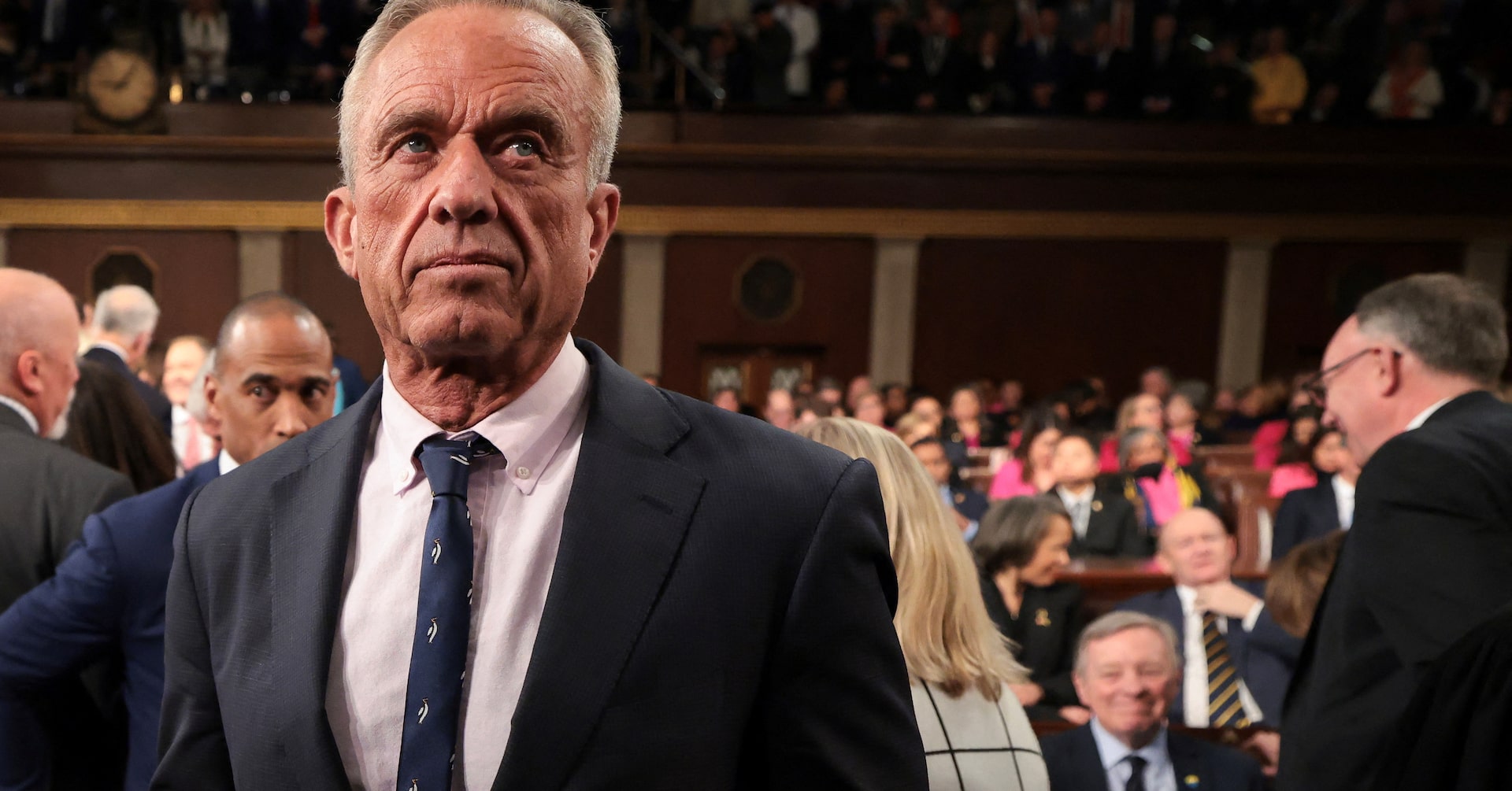
Nutrition Showdown: Health Secretary Kennedy Summons Food Industry Leaders for Urgent Talks
2025-03-08 14:43:46