Dark Shadows at Sanctuary: Systemic Failures Expose Mental Health Center's Hidden Crisis
Health
2025-04-22 09:00:32Content

In the quiet suburbs of Lemont, Illinois, Timberline Knolls stood as a beacon of hope for women and girls struggling with mental health and addiction. Owned by Acadia Healthcare, the residential treatment center promised healing and recovery. But beneath its serene exterior, a troubling pattern of understaffing and systemic neglect was brewing—a situation that would soon lead to devastating consequences.
The facility, which prided itself on treating complex mental health conditions, was chronically short-staffed. Overworked employees were stretched thin, struggling to provide the comprehensive care patients desperately needed. This dangerous cost-cutting approach created an environment where vulnerable individuals were at significant risk.
What followed was a heartbreaking series of tragedies that exposed the critical gaps in the center's care model. Patient safety became secondary to operational efficiency, with potentially fatal consequences. Each incident shed light on a deeper, more systemic problem: a healthcare system that prioritized profits over patient well-being.
The stories that emerged were not just statistics, but deeply personal accounts of lives put in jeopardy. Young women seeking help found themselves in an environment that was supposed to heal but instead potentially endangered their recovery and safety.
As investigations unfolded, the stark reality became clear: Timberline Knolls' staffing shortcuts were not just an administrative failure, but a profound breach of the fundamental trust patients and their families place in mental health treatment centers.
Unraveling the Crisis: Mental Health Care Failures at Timberline Knolls Exposed
In the complex landscape of mental health treatment, institutions are entrusted with the most vulnerable members of society, bearing an immense responsibility that extends far beyond mere medical care. The story of Timberline Knolls, a mental health facility owned by Acadia Healthcare, reveals a deeply troubling narrative of systemic negligence that threatens the very foundation of patient safety and therapeutic recovery.When Understaffing Becomes a Deadly Compromise
The Institutional Breakdown of Patient Care
Timberline Knolls represents a microcosm of broader challenges plaguing mental health treatment centers across the United States. The facility's chronic understaffing created a perfect storm of potential catastrophic outcomes, where patient vulnerability intersected with institutional resource constraints. Mental health professionals understand that adequate staffing isn't just a logistical concern—it's a critical lifeline for individuals navigating complex psychological landscapes. The implications of insufficient personnel extend far beyond mere operational inefficiencies. Each staff member represents a potential intervention point, a critical connection between patient safety and therapeutic progress. When these positions remain unfilled, the entire ecosystem of care becomes fundamentally compromised, creating environments where risk escalates exponentially.Systemic Failures in Mental Health Infrastructure
The challenges at Timberline Knolls illuminate broader systemic issues within mental health care delivery. Understaffing isn't an isolated incident but a symptom of deeper structural problems that permeate healthcare institutions. Financial constraints, regulatory gaps, and persistent workforce shortages contribute to an environment where patient safety becomes increasingly precarious. Healthcare experts argue that these institutional failures represent more than administrative oversights—they reflect a profound societal neglect of mental health infrastructure. The human cost of such negligence is immeasurable, with each understaffed shift potentially representing missed opportunities for intervention, support, and healing.The Human Toll of Institutional Negligence
Behind every statistic and administrative report are real human experiences—individuals seeking refuge, healing, and hope. The tragedies emerging from Timberline Knolls aren't abstract data points but deeply personal narratives of suffering exacerbated by systemic failures. Mental health treatment demands more than clinical protocols; it requires a holistic, compassionate approach that recognizes the intricate psychological landscapes of patients. When institutions prioritize cost-cutting over comprehensive care, they fundamentally betray the core ethical principles of healthcare.Accountability and Institutional Transformation
The revelations surrounding Timberline Knolls demand comprehensive accountability. Regulatory bodies, healthcare administrators, and policymakers must recognize that understaffing isn't merely an operational challenge but a critical patient safety issue. Transformative change requires multi-dimensional strategies: improved funding mechanisms, robust staffing standards, enhanced professional training programs, and stringent oversight protocols. Only through systematic, holistic approaches can mental health institutions begin to rebuild trust and ensure genuine therapeutic environments.The Broader Implications for Mental Health Care
The Timberline Knolls narrative serves as a powerful cautionary tale, challenging healthcare stakeholders to reevaluate existing paradigms of mental health treatment. It underscores the urgent need for a fundamental reimagining of institutional care models, prioritizing human dignity, comprehensive support, and genuine healing over narrow economic considerations. As society continues to grapple with increasing mental health challenges, the lessons from Timberline Knolls must not be forgotten. They represent a critical call to action, demanding sustained commitment to transforming mental health care from a potentially dangerous system to a genuinely supportive, life-affirming ecosystem of care.RELATED NEWS
Health

Breaking: Apalachee Head Coach Prioritizes Personal Well-being, Steps Away from Sidelines
2025-03-03 22:54:11
Health
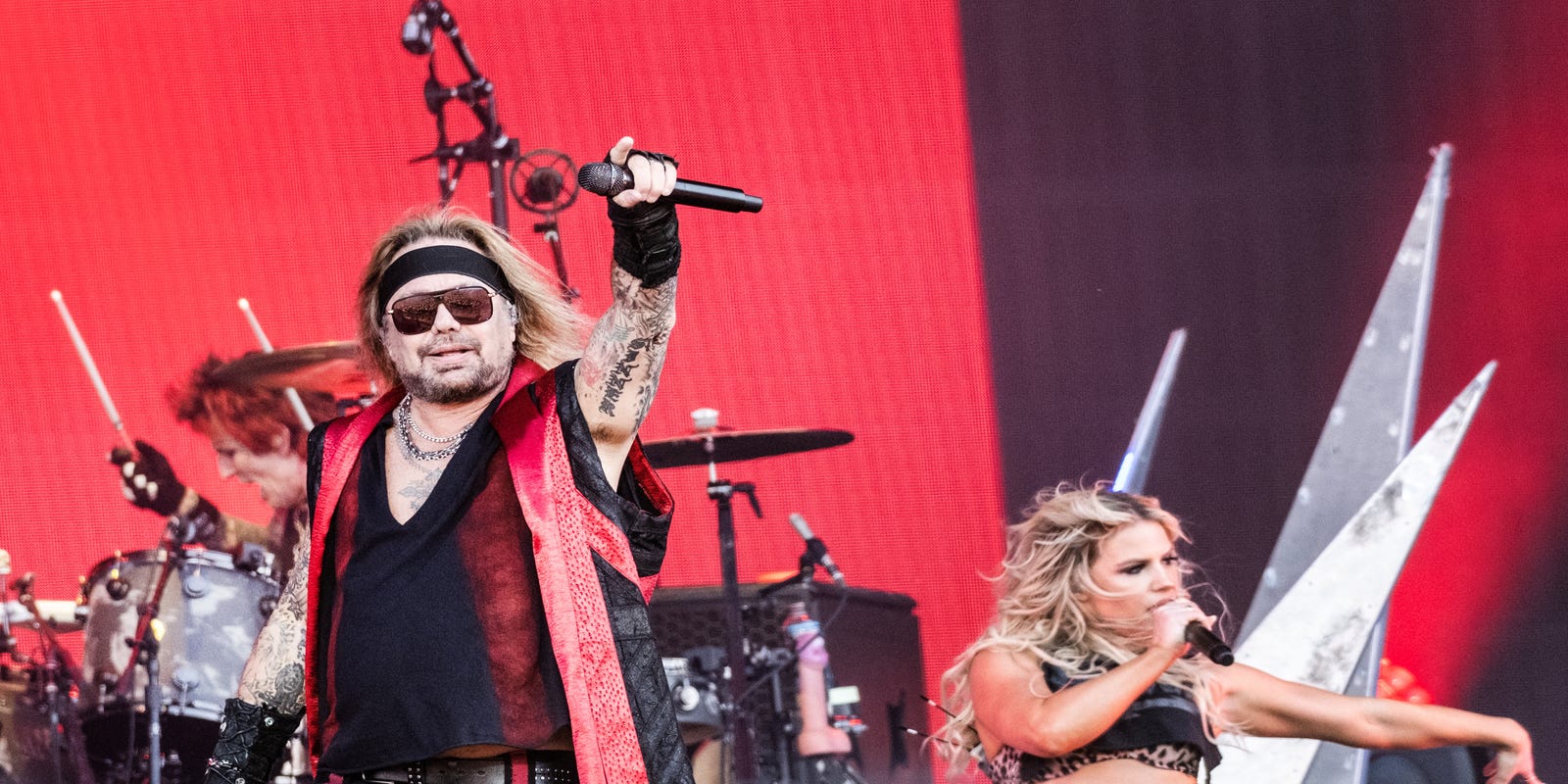
Rock Chaos: Mötley Crüe Halts Vegas Residency After Vince Neil's Unexpected Medical Setback
2025-03-04 23:25:15
Health

Behind the Tragedy: Nashville Shooter's Hidden Struggles and Quest for Infamy
2025-04-02 16:21:22





