Behind Closed Doors: The Hidden Crisis in Children's Mental Health Care
Health
2025-04-11 12:29:51Content

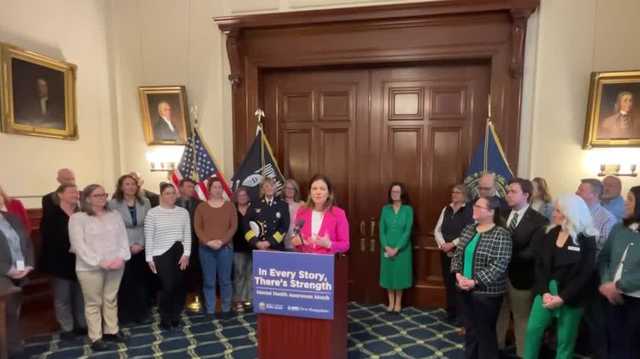
Mental Health Advocacy Takes Center Stage: Key Healthcare Challenges Highlighted
The Missouri Hospital Association (MHA) captured media attention during the week of April 7, shedding light on critical healthcare issues that are impacting communities statewide. Focusing on three pivotal areas - potential Medicaid funding reductions, pediatric behavioral health challenges, and escalating healthcare costs - the organization brought important conversations to the forefront of public discourse.
Journalists and healthcare professionals alike were drawn to the MHA's comprehensive analysis, which underscored the potential consequences of proposed funding cuts and the urgent need for sustainable healthcare solutions. The discussion emphasized the delicate balance between financial constraints and maintaining quality patient care, particularly for vulnerable populations such as children with behavioral health needs.
By bringing these complex issues into the media spotlight, the MHA continues to play a crucial role in advocating for healthcare accessibility, affordability, and quality across Missouri. Their proactive approach ensures that critical healthcare challenges remain a priority for policymakers and the public.
Healthcare Horizons: Navigating the Complex Landscape of Medicaid, Pediatric Care, and Rising Medical Expenses
In the ever-evolving world of healthcare, critical challenges continue to reshape the landscape of medical services, funding, and patient care. As policymakers, healthcare providers, and community organizations grapple with increasingly complex systemic issues, the intersection of Medicaid, pediatric behavioral health, and escalating healthcare costs demands unprecedented attention and innovative solutions.Unraveling the Critical Challenges in Modern Healthcare Delivery
The Medicaid Funding Conundrum: A Delicate Balance of Resources and Need
The potential Medicaid funding cuts represent a seismic shift in healthcare accessibility that could fundamentally transform medical support for vulnerable populations. Healthcare experts warn that these proposed reductions could create devastating ripple effects across community health networks. Comprehensive analysis reveals that such cuts would not merely represent a budgetary adjustment, but a potential humanitarian crisis affecting millions of low-income individuals and families. Deeper investigations suggest that these funding modifications stem from complex economic pressures and political negotiations. State-level administrators are confronting unprecedented challenges in maintaining robust healthcare infrastructure while managing increasingly constrained financial resources. The potential implications extend far beyond immediate budget considerations, potentially undermining long-term public health strategies and community wellness initiatives.Pediatric Behavioral Health: Addressing the Silent Crisis
The emerging landscape of pediatric behavioral health demands immediate and comprehensive intervention. Mental health challenges among children and adolescents have reached critical levels, exacerbated by pandemic-induced social disruptions and increasing psychological pressures. Healthcare professionals are witnessing an unprecedented surge in mental health diagnoses, highlighting the urgent need for specialized, accessible support systems. Innovative approaches are emerging that integrate holistic care models, combining psychological assessment, family support, educational interventions, and targeted therapeutic strategies. These multifaceted approaches recognize the complex interconnections between mental health, social environments, and developmental trajectories. By reimagining pediatric behavioral health support, healthcare providers aim to create more responsive, compassionate, and effective treatment frameworks.The Rising Tide of Healthcare Costs: Economic Pressures and Patient Challenges
Healthcare expenditures continue to escalate at an alarming rate, creating significant economic strain for individuals, families, and institutional providers. The intricate web of medical pricing, insurance complexities, and technological advancements contributes to a healthcare ecosystem that feels increasingly unsustainable for many Americans. Economists and healthcare policy experts are exploring multifaceted strategies to mitigate these rising costs. Potential solutions range from implementing transparent pricing mechanisms to developing innovative insurance models that prioritize preventative care and patient-centered approaches. The goal extends beyond mere cost reduction, focusing on creating a more equitable, accessible healthcare system that balances economic sustainability with comprehensive medical support.Interconnected Challenges: A Holistic Perspective on Healthcare Transformation
The convergence of Medicaid funding challenges, pediatric behavioral health needs, and escalating healthcare costs represents a critical moment of potential systemic transformation. Healthcare stakeholders are increasingly recognizing the necessity of integrated, collaborative approaches that transcend traditional institutional boundaries. Emerging research suggests that comprehensive, patient-centered strategies offer the most promising path forward. By prioritizing holistic care models, leveraging technological innovations, and developing adaptive policy frameworks, healthcare systems can potentially create more resilient, responsive, and equitable medical support networks.RELATED NEWS
Health

Healing Hearts: Pope Praises Volunteers' Compassion as Medical Team Signals Promising Recovery
2025-03-09 14:06:53
Health

Finding Healing: Essentia Health Launches Compassionate Grief Support Sessions
2025-03-02 22:00:00
Health

Bonus Bombshell: Mental Health Executives' Lucrative Incentives Amid Federal Probe
2025-04-24 09:01:55